Most healthcare systems still rely on fragmented tools that slow down operations and create unnecessary complexity. Administrative work piles up, critical data stays locked in outdated systems, and care teams struggle to deliver connected experiences that patients now expect.
Healthcare SaaS platforms provide scalable, secure, and compliant solutions that streamline clinical operations, eliminating the need for extensive hardware or lengthy deployments. Cloud delivery enables faster implementation, real-time access, and smoother integration across systems that need to work together.
This blog explores how SaaS is changing the way healthcare organizations manage operations and deliver care. It covers practical applications, key benefits, common challenges, and what to look for in a SaaS provider that understands both clinical workflows and compliance demands.
Key Takeaways
- Healthcare SaaS enhances care delivery, streamlines operations, and reduces reliance on outdated infrastructure.
- Core applications include EHRs, telehealth platforms, practice management tools, analytics systems, and lab software.
- Common implementation barriers involve compliance complexity, integration issues, user resistance, and limited internal capacity.
- Future trends include AI-powered diagnostics, modular microservices, advanced API ecosystems, and predictive analytics.
- Organizations that act early can build scalable systems, improve data visibility, and support proactive care models.
What SaaS Means for the Healthcare Industry
Software-as-a-Service (SaaS) delivers applications over the cloud, removing the need for hospitals and clinics to manage on-premise servers, manual upgrades, or infrastructure maintenance. Instead of lengthy IT cycles and substantial hardware investments, healthcare teams can access secure, compliant software through a browser or mobile app.
In healthcare, SaaS addresses critical delivery issues, including fragmented patient data, limited care coordination, and rising operational costs. Care teams can access records remotely, coordinate across locations in real time, and roll out new features without disrupting the system.
The flexibility of SaaS aligns with the complex operational structures of the healthcare industry. Multi-location systems, specialty clinics, and diagnostic labs can all configure workflows, permissions, and dashboards to match their specific needs. Cloud-native platforms scale with demand, adapt to usage patterns, and integrate with existing tools using standards such as HL7 FHIR.
SaaS also supports faster deployment for new medical technologies. With compliance frameworks built in, covering HIPAA, GDPR, and regional mandates, organizations can launch securely from day one.
Key Benefits of Healthcare SaaS for Modern Organizations
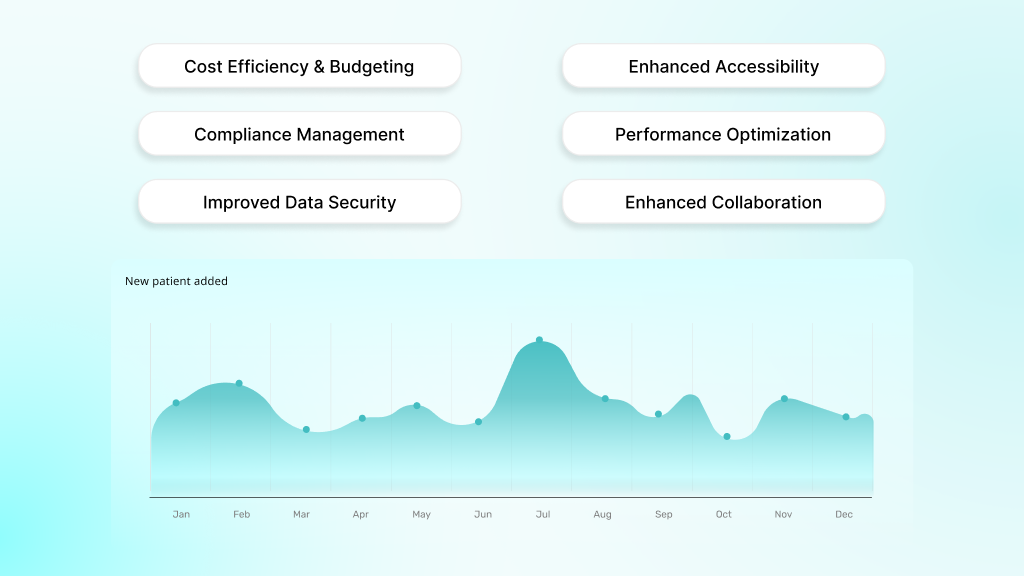
The value of SaaS in healthcare primarily stems from operational control. It eliminates the overhead of maintaining infrastructure, simplifies compliance, and provides teams with the flexibility to scale without requiring system rework each time.
In this section, we will break down how these benefits apply across costs, workflows, and care delivery.
Cost Efficiency and Predictable Budgeting
SaaS subscription models eliminate the need for large upfront capital expenditures on hardware and software licenses. Instead, healthcare organizations pay predictable monthly fees that cover infrastructure, maintenance, security updates, and technical support.
Since cloud infrastructure scales automatically based on usage, teams can avoid over-provisioning and underutilization. This flexibility leads to more efficient resource allocation and helps reduce overall IT costs.
Enhanced Accessibility and Mobility
With cloud-based platforms, healthcare providers can access patient records and complete clinical tasks from any location. They can review charts during home visits, update notes from mobile devices, and stay connected to critical systems without relying on on-site servers.
Mobile applications support bedside consultations and remote care delivery, maintaining secure connections through encrypted VPN tunnels. This level of access improves responsiveness, expands coverage, and contributes to better work-life balance for providers.
Automatic Updates and Compliance Management
Staying compliant in healthcare requires constant alignment with shifting regulations and security standards. SaaS platforms take full ownership of this responsibility by delivering automatic updates across all instances without requiring action from internal teams.
Compliance protocols are built into the system and adjusted as policies evolve, reducing the risk of gaps or delays. This keeps providers focused on care delivery while ensuring their technology environment consistently meets current regulatory expectations.
Scalability and Performance Optimization
Cloud-based SaaS platforms scale with healthcare organizations as they grow. Adding users, deploying new features, or expanding to new locations does not require costly infrastructure upgrades or system migrations.
Performance remains consistent across high-demand periods. Most platforms include monitoring tools to ensure that application response times remain under two seconds, even during periods of peak usage, thereby maintaining a seamless user experience.
Improved Data Security and Backup
Enterprise-grade security is built into leading SaaS platforms. Features such as AES-256 encryption, role-based access controls, and complete audit logging protect sensitive medical data at every layer.
Automated backup systems safeguard information against accidental loss, while disaster recovery protocols ensure business continuity. Most platforms ensure high uptime and offer greater reliability than many organizations can maintain with in-house systems.
Enhanced Collaboration and Communication
SaaS enables real-time collaboration across departments, facilities, and specialties. Care teams can access shared records instantly, allowing for faster decision-making and reduced administrative delays.
By unifying clinical data across the system, duplicate testing is reduced, while integrated messaging and alerts support secure communication. All communication remains HIPAA-compliant, even across mobile and remote workflows.
Where Healthcare SaaS Delivers the Most Impact
SaaS platforms now support critical operations across the healthcare system, from clinical documentation to lab reporting. These solutions not only reduce delays and errors but also strengthen coordination across departments.
Here is how different applications deliver real, measurable improvements.
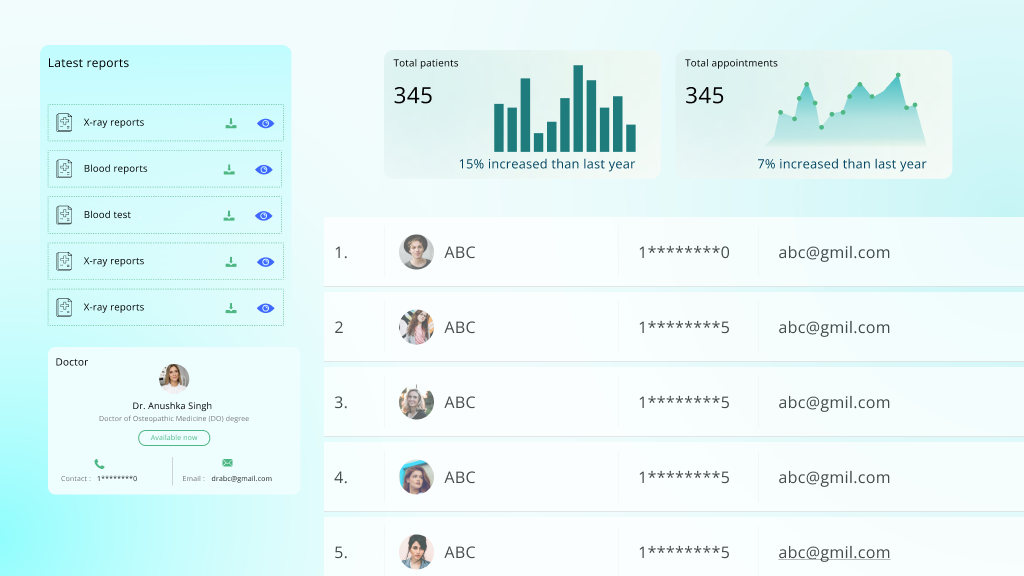
Electronic Health Records (EHR)
Cloud-based EHR systems keep patient data accessible, organized, and secure. Care teams can review complete medical histories, lab results, and treatment plans from any connected device. Built-in clinical decision support helps reduce prescription errors by up to 55 percent. Integrated billing tools improve cash flow by simplifying revenue cycle management.
Telehealth and Virtual Care Tools
Modern telehealth platforms use SaaS infrastructure to enable secure video visits, encrypted messaging, and real-time monitoring. Connected devices and IoT wearables track vitals and chronic conditions between appointments. Providers can serve more patients remotely while reducing travel and wait times. Many clinics report a substantial increase in service capacity with these tools in place.
Medical Practice Management Systems
SaaS-based practice management tools automate routine front-desk tasks, such as scheduling, insurance verification, and patient communication. Automated reminders and built-in billing features reduce errors and delays, enabling teams to get paid faster and stay focused on what matters.
Healthcare Analytics Platforms
Analytics platforms built on SaaS architecture make it easier to spot trends and make informed decisions. Clinical analytics support better treatment planning and outcome tracking. Population health tools segment patients by risk or condition, allowing earlier interventions. Financial modules utilize predictive modeling to optimize resource allocation and pinpoint revenue gaps.
Laboratory Information Systems (LIS)
Cloud-based LIS platforms bring speed and structure to lab operations. They manage specimen tracking, test ordering, and result delivery through automated workflows. Results sync with EHRs and appear in patient records within 15 minutes of completion. Quality controls catch issues early, while built-in compliance tools help labs maintain CLIA and CAP certifications.
Challenges That Slow Healthcare SaaS Adoption
While SaaS platforms offer clear advantages to the healthcare industry, their implementation is not without its challenges. Beginning with compliance gaps and legacy infrastructure, the path to modernization presents real barriers. Listed below are some of the most common challenges and their effective management strategies.
Compliance Gaps in Cloud Environments
SaaS platforms must align with complex data protection laws, such as HIPAA and GDPR, as well as regional mandates. Without proper controls, even a slight lapse in how patient data is stored or accessed can result in penalties, audits, or a loss of trust.
How to prevent it
Work with SaaS providers that can prove their compliance posture. Look for SOC 2 Type II, HITRUST, and other relevant certifications. Request documented practices regarding encryption, access control, and breach response. For international operations, ensure your provider can enforce jurisdictional compliance across data zones.
Resistance from Legacy Systems
Many healthcare organizations still rely on proprietary legacy systems that were not built for interoperability. These systems create data silos and resist cloud integration. Migrating from them often reveals inconsistencies, unsupported formats, or outdated workflows.
How to prevent it
Adopt a phased rollout. Maintain legacy and cloud systems in parallel for a specified transition period. Choose a SaaS vendor with hands-on experience in FHIR and HL7 integration. Ensure they can support data migration and system alignment without operational downtime.
Inconsistent Data Integration and Shadow IT
Data originates from multiple sources in healthcare, including EHRs, labs, medical devices, external portals, and apps. When departments bypass IT and use tools without approval, it creates shadow IT risks. These unmonitored tools increase the chance of data leaks and non-compliance.
How to prevent it
Implement strict governance over all cloud-based tools and services. Utilize a cloud access security broker (CASB) to monitor usage and enforce access controls throughout the organization. Conduct regular penetration testing to identify weak points before they become critical.
Low User Adoption and Workflow Disruption
Clinicians are often resistant to tools that interrupt their established workflows. If the new system is unintuitive or slows them down, adoption suffers. Productivity drops, and confidence in the platform erodes quickly.
How to prevent it
Provide training tailored to each user group. Prioritize usability during vendor selection. Roll out the tool in phases, starting with pilot teams. Assign internal champions who can support others and share honest user feedback with implementation teams.
Limited Internal Capacity for Full Deployment
Some organizations struggle to allocate internal resources for configuration, training, and long-term support. Without a dedicated team, SaaS adoption may stall or remain underutilized.
How to prevent it
Partner with a provider like DEVtrust, as they understand the healthcare environment and offer hands-on support beyond the software itself. They work closely with internal teams to manage compliance, configure systems, and deliver custom features that align with clinical operations. Schedule a consultation to discuss your requirements with a team that has experience in building healthcare solutions.
The Future of SaaS in Healthcare Technology
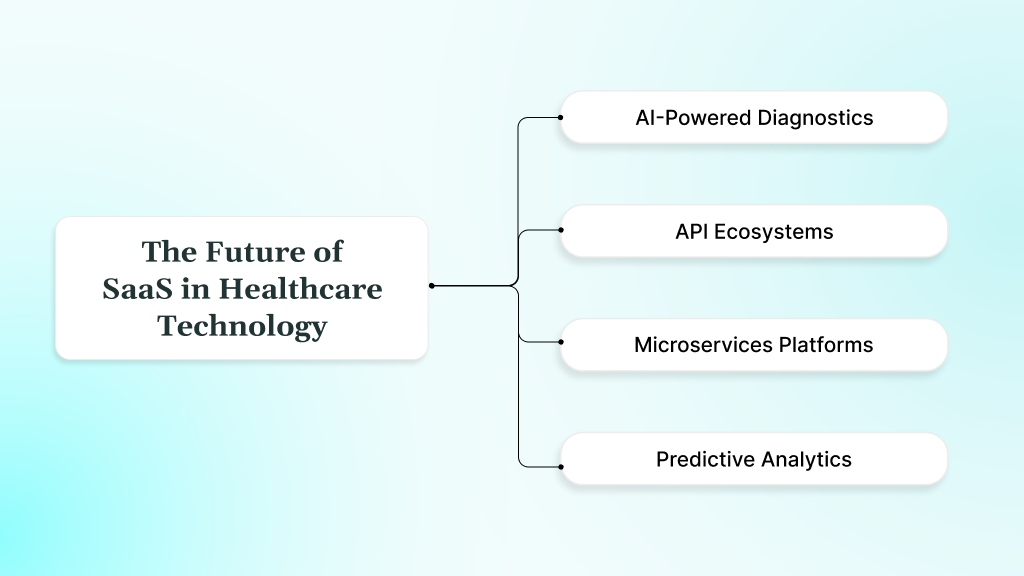
SaaS in healthcare is moving toward more intelligent, modular, and connected systems. What started as a way to replace on-premise software is now driving real change in how care is delivered, documented, and scaled.
Here is where the future is heading and what it means for healthcare organizations making decisions today.
AI-Powered Diagnostics and Workflow Automation
SaaS platforms are advancing beyond record management to support clinical decisions actively. Integrated AI tools analyze patient data to identify early warning signs, highlight potential risks, and suggest targeted interventions based on a patient’s clinical history. This improves diagnostic accuracy and supports faster response times.
Documentation is becoming less of a burden as well. Voice-based inputs, automatic transcription, and natural language processing are helping doctors save time without compromising accuracy. These tools integrate directly with SaaS EHRs and practice management systems, streamlining workflows without the need for separate systems.
API Ecosystems
System-level integration is now built into modern SaaS platforms. Through connected APIs, data is transmitted securely across providers, payers, labs, and medical devices, eliminating the need for manual steps or delays. Insurers can view treatment updates in real time, and patient vitals stream directly from devices into the tools used by care teams.
Behind this is the broader adoption of FHIR standards, which make data exchange more structured and secure across different vendors. With cleaner interoperability in place, care teams can reduce administrative layers and deliver better-coordinated treatment without having to work across siloed systems.
Microservices-Based Modular SaaS Platforms
Healthcare teams are shifting away from monolithic platforms that attempt to encompass everything in a single system. Instead, they are adopting modular SaaS tools that address specific functions, clinical documentation, patient scheduling, billing, or reporting, and integrating only what fits their workflow.
With containerized deployments and microservices, these tools can perform reliably across environments while allowing for adaptation. This setup helps growing networks and smaller clinics build systems that align with their actual operations, without overspending on features they do not need.
Predictive Analytics and Population Health Management
Cloud-based SaaS platforms are making it easier to turn raw healthcare data into actionable insight. With predictive analytics, care teams can identify high-risk patients earlier, allocate resources more efficiently, and anticipate trends in the management of chronic conditions.
Real-time data processing supports continuous monitoring, instant alerts, and long-term analysis across patient groups. This shift allows healthcare organizations to move beyond reactive care and adopt more proactive, prevention-led approaches that reduce emergency interventions and improve long-term outcomes.
How to Choose the Right SaaS Provider for Your Healthcare Organization
Healthcare organizations face mounting pressure to modernize their legacy systems while ensuring data security, maintaining patient trust, and complying with regulations. With sensitive patient data at stake and the complexity of medical workflows, selecting the wrong SaaS partner can result in compliance gaps, system failures, and costly setbacks.
An effective SaaS provider does more than offer software. It must understand the clinical environment, enable secure integrations, and adapt to shifting needs without compromising reliability or uptime.
What Makes a Healthcare SaaS Partner Worth Trusting
Evaluating a SaaS partner requires more than checking features. The real difference shows in how well they support your goals, adapt to your systems, and hold up over time. Look for these qualities during evaluation:
- Healthcare-Specific Knowledge: Familiarity with patient engagement, clinical data flows, and hospital administration tools is essential. A capable partner should reflect a history of working with healthcare teams, not just generic software deployments.
- Privacy and Security-Centric Architecture: The partner should prioritize patient data safety by implementing strong encryption protocols, secure user authentication layers, and infrastructure that supports strict access management.
- Customization and Integration Support: Every healthcare operation has different needs. Ensure the partner can tailor workflows, integrate with medical APIs, and scale as your patient or provider network grows.
- Responsive Support and Implementation Guidance: Smooth onboarding, post-launch assistance, and a clear escalation path are non-negotiable. Timely support can make the difference between clinical disruption and smooth continuity.
What the Right Partner Delivers in Practice
The best-fit partner builds for real-world constraints in healthcare, balancing compliance with speed, and custom logic with stability. They maintain open communication with stakeholders, understand the risks associated with downtime, and adapt their delivery to suit both legacy infrastructure and emerging health tech trends.
They bring full-stack knowledge across backend systems, cloud platforms, and patient-facing interfaces. This expertise spans virtual care and in-clinic platforms, all while upholding strong standards for security and interoperability.
Where DEVtrust Fits In
DEVtrust applies these principles across all healthcare engagements. Their engineers understand the demands of building platforms that support secure patient communication, clinical workflows, and environments that are sensitive to regulatory requirements.
Their experience encompasses EHR systems, telemedicine platforms, and AI-assisted documentation tools utilized across clinics, therapy practices, and insurance technology. These tools are built to integrate with APIs like Zoom Health, Azure Health, and Twilio, ensuring everything connects within the care ecosystem.
In a recent engagement with Spero Institute, DEVtrust delivered a custom platform that addressed key operational and clinical needs:
- Secure role-based access for clinicians and patients
- Streamlined document management to simplify record storage and retrieval
- Visual DBT progress tracker to monitor therapy outcomes over time
- Built-in scheduling and messaging to coordinate care seamlessly
- Integrated video conferencing to support remote sessions and virtual visits
- Protected data flows through secure login protocols and access control layers.
The platform improved coordination between therapists and patients, enhanced data security, and gave Spero’s team visibility into client progress, all within a tailored, compliant system.
Conclusion
SaaS has become a practical choice for healthcare organizations looking to improve system performance without adding complexity. It supports faster delivery, simpler maintenance, and long-term adaptability. This makes it a strong fit for the demands of modern care environments.
EHR systems, telehealth platforms, lab management tools, and AI-powered documentation solutions now depend on flexible SaaS architectures that support real-time access, secure integrations, and continuous updates. Healthcare organizations that invest in the right SaaS strategy will gain measurable advantages.
Contact us if you are looking to build secure, purpose-driven SaaS platforms with the right strategy for your healthcare operations.
How Healthcare SaaS Is Shaping Technology in 2025
Discover how healthcare SaaS streamlines operations, enhances patient care, and ensures secure, scalable solutions. Explore future trends now!
Contact Us