In 2025, the global electronic health record (EHR) market is projected to reach USD 41 billion, driven by increasing demand for digital healthcare solutions and regulatory mandates for interoperability. As a healthcare provider or developer, building a custom EHR system offers you the opportunity to streamline clinical workflows, enhance patient care, and stay ahead in a rapidly evolving industry.
This guide provides a comprehensive roadmap for developing EHR software, detailing essential features, compliance requirements, technology choices, and cost estimates tailored for 2025.
You’ll learn the step-by-step process to create a reliable EHR system, understand the challenges, and incorporate future trends such as AI and blockchain. With practical insights, this guide helps you to build a solution that meets the needs of clinics, hospitals, and patients.
Key Takeaways
- EHR software digitizes patient records, differing from EMR by supporting interoperability across systems.
- Custom EHRs offer scalability and integration with AI, telehealth, and wearables in 2025.
- Prioritize HIPAA, GDPR, and ONC compliance with encryption and role-based access.
- Use tech stacks like React, Node.js, and FHIR for modern, scalable EHRs.
- Plan for $80K-$150K for an MVP, with full solutions costing $250K+.
What Is EHR Software?
EHR software is a digital platform that stores and manages patient health information, enabling secure access and sharing across healthcare providers. Unlike electronic medical records (EMRs), which are limited to a single organization’s data, EHRs support interoperability, allowing data exchange between clinics, hospitals, and labs. You can deploy EHRs as web-based systems (cloud-hosted), on-premise (local servers), or hybrid models combining both. Benefits include streamlined workflows for clinics, faster decision-making for hospitals, and improved access for patients via portals.
Understanding EHRs sets the stage for exploring why a custom solution is valuable in 2025.
Why Develop a Custom EHR in 2025?
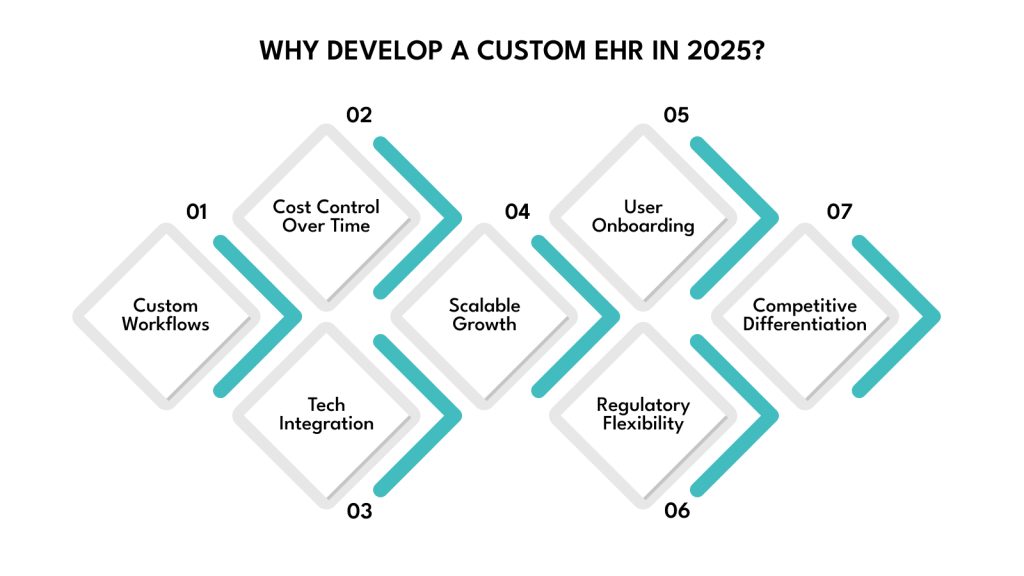
Building a custom electronic health record (EHR) system in 2025 offers you a tailored solution to meet the unique needs of your healthcare organization, overcoming the limitations of off-the-shelf software. Pre-built EHRs, such as Epic or Cerner, often come with rigid workflows, high licensing fees, and limited flexibility, which can hinder efficiency in clinics or hospitals with specific requirements.
A custom EHR allows you to design a system that aligns perfectly with your clinical processes, integrates seamlessly with emerging technologies, and scales as your organization grows. Here are some reasons why you should develop a custom EHR:.
- Tailored Workflows for Specific Needs: Customize your EHR to match the workflows of your clinic or hospital, such as specialized charting for cardiology or streamlined billing for small practices, improving efficiency and reducing staff frustration compared to one-size-fits-all solutions.Traditional EHR systems often burden clinicians with excessive clicks and fragmented data views. In contrast, well-designed custom systems can significantly reduce documentation fatigue. In fact, studies show that EHR adoption can reduce documentation time by 22.4%, streamlining workflows and lowering administrative burden for healthcare providers.
- Cost Control Over Time: Avoid recurring licensing fees of off-the-shelf EHRs, which can cost $10,000-$50,000 annually for mid-sized practices. A custom EHR involves upfront investment but reduces long-term costs through tailored maintenance and updates.
- Seamless Integration with Modern Technologies: Build your EHR to connect with wearables, AI-driven diagnostics, or telehealth platforms, ensuring compatibility with 2025’s tech trends, unlike pre-built systems that may lag in supporting new tools.
- Enhanced Scalability for Growth: Design a modular system that scales with your organization, adding features like patient portals or analytics as needed, without the constraints of vendor-locked software.
- Improved User Adoption: Create intuitive interfaces that align with clinician preferences, reducing training time and resistance compared to generic EHRs that often overwhelm users with complex navigation.
- Regulatory Flexibility: Embed compliance with evolving regulations like HIPAA or NDHM directly into your system, allowing quicker adaptations to 2025’s regulatory changes without waiting for vendor updates.
- Competitive Differentiation: Offer unique features, like AI-powered insights or patient-focused apps, to attract healthcare providers seeking innovative solutions, setting your organization apart in a crowded market.
With the advantages of custom development clear, let’s examine the essential features your EHR should include.
Key Features of Modern EHR Software
A modern EHR system must balance core functionalities with advanced features to meet clinical and patient needs in 2025. You’ll need to prioritize features that enhance usability, efficiency, and compliance while incorporating innovative tools to stay ahead in healthcare.
Core Features
Your EHR should include foundational features to support clinical operations. Here are some of them:
- Patient Records and Charting: Store and update comprehensive patient histories, including diagnoses, allergies, and treatment plans, with real-time access for clinicians.
- Appointment Scheduling: Enable easy booking with calendar integrations, automated reminders, and conflict detection to optimize clinic workflows.
- E-Prescriptions: Support digital medication orders with integration to pharmacies, reducing errors and speeding up prescription fulfillment.
- Lab and Imaging Integrations: Connect with diagnostic systems to retrieve and store lab results or imaging reports seamlessly within patient records.
- Billing, Claims, and Insurance: Automate billing processes, submit insurance claims, and track reimbursements to ensure financial accuracy and efficiency.
Advanced Features
Incorporate these cutting-edge features to enhance functionality and align with 2025’s healthcare trends.
- Clinical Decision Support (AI): Use AI to analyze patient data and suggest diagnoses, treatment plans, or risk alerts, improving clinical outcomes.
- Voice-Enabled Documentation: Enable speech-to-text charting to speed up documentation, allowing clinicians to focus more on patient care.
- Telehealth Modules: Integrate virtual consultation tools for remote patient visits, supporting video calls and secure messaging.
- Patient Portal and Mobile Apps: Provide patients with secure access to their records, appointment scheduling, and communication via web or mobile platforms.
- Real-Time Compliance Alerts: Notify staff of regulatory updates or potential compliance issues, such as missing HIPAA documentation, to ensure adherence.
With features defined, let’s explore the compliance and security standards critical for EHR development.
Compliance and Security Standards (2025 Update)
Compliance with regulations and robust security practices is non-negotiable for EHR software, as they protect sensitive patient data and ensure legal adherence. In 2025, evolving standards demand careful attention to safeguard your system and maintain trust.
Major Regulations
Your EHR must adhere to global and regional regulations to ensure data protection and interoperability. Below are the primary regulations you need to address:
- HIPAA (Health Insurance Portability and Accountability Act): A U.S. law requiring secure handling of protected health information (PHI), mandating encryption, access controls, and patient consent to prevent unauthorized access and ensure privacy.
- GDPR (General Data Protection Regulation): A European regulation governing personal data, requiring explicit user consent, data minimization, and the right to data erasure, applicable to EHRs handling EU patient data.
- NDHM (National Digital Health Mission): India’s framework for digital health records, emphasizing interoperable EHRs, patient consent, and secure data sharing across healthcare providers.
- PIPEDA (Personal Information Protection and Electronic Documents Act): Canada’s privacy law, mandating secure data collection, storage, and user consent for health data, with strict breach reporting requirements.
- ONC Certification (Office of the National Coordinator for Health Information Technology): A U.S. program ensuring EHRs meet interoperability and functionality standards, requiring support for FHIR and patient data access.
Essential Security Practices
Implement these security measures to protect your EHR and ensure compliance with the above regulations.
- Data Encryption: Use AES-256 encryption for data at rest and TLS for data in transit to secure patient information against breaches.
- Role-Based Access Control (RBAC): Restrict access to authorized users, such as doctors or admins, based on their roles to prevent unauthorized data viewing.
- Audit Trails: Maintain detailed logs of all system access and data changes to support compliance audits and track potential security incidents.
- Multi-Factor Authentication (MFA): Requires multiple verification steps, like passwords and biometrics, to secure user logins and reduce unauthorized access risks.
- Privacy-by-Design: Embed privacy principles into development, such as minimizing data collection and anonymizing PHI, to align with regulations from the start.
With compliance addressed, let’s select the technology stack to build your EHR system.
Technology Stack for EHR Software Development
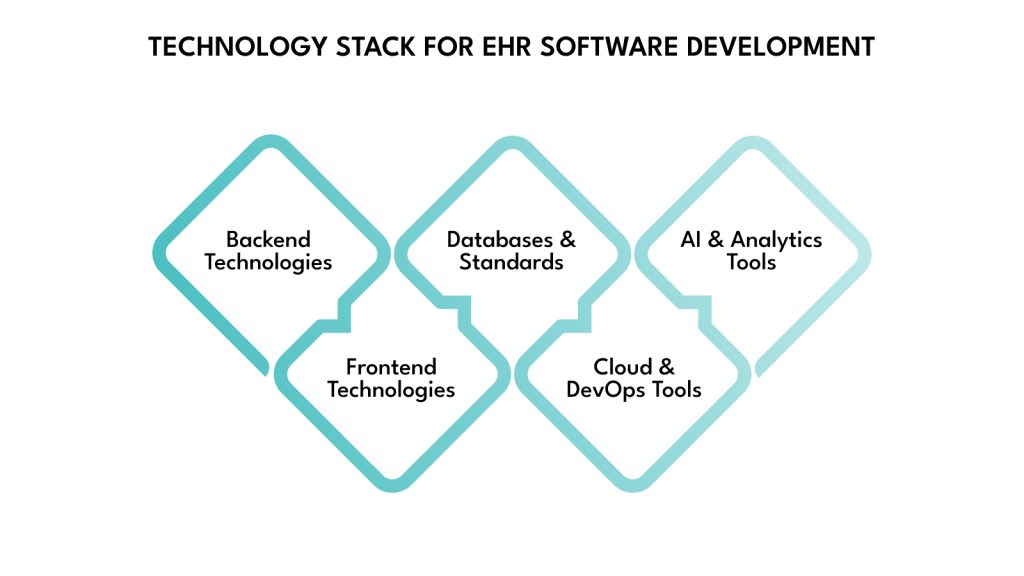
Choosing the right technology stack ensures your EHR is scalable, secure, and efficient. You need tools that support complex healthcare data, comply with standards, and enable modern features like AI and telehealth. This section outlines recommended technologies for 2025.
Backend Technologies
Node.js with Express offers fast, scalable server-side logic for real-time data. Python with Django or Flask provides robust frameworks for secure, healthcare-focused applications. Java Spring Boot excels for enterprise-grade systems, ensuring reliability and scalability for large hospitals.
- Options: Node.js, Django/Flask, Java Spring Boot.
- Why They Matter: Handle complex logic and ensure performance.
Frontend Technologies
React provides a responsive, component-based UI for patient portals and dashboards. Angular offers structured development for large-scale apps. Vue.js balances simplicity and flexibility, ideal for smaller clinics needing clean interfaces.
- Options: React, Angular, Vue.js.
- Why They Matter: Create intuitive, user-friendly interfaces.
Databases and Standards
PostgreSQL supports structured data like patient records, ensuring reliability. MongoDB handles flexible, unstructured data like imaging results. Use HL7, FHIR, and SMART on FHIR standards for interoperability, enabling seamless data exchange between healthcare systems.
- Options: PostgreSQL, MongoDB, HL7/FHIR standards.
- Why They Matter: Ensure data integrity and interoperability.
Cloud & DevOps Tools
AWS, Azure, or GCP provide secure, scalable cloud hosting with HIPAA-compliant options. Docker containerizes your app for consistent deployment, while Kubernetes manages scaling for high-traffic systems, ensuring uptime during peak usage.
- Options: AWS, Azure, GCP, Docker, Kubernetes.
- Why They Matter: Support scalability and compliance.
AI & Analytics Tools
TensorFlow or PyTorch power AI-driven features like clinical decision support. Power BI or Tableau visualize patient data trends, helping clinicians make informed decisions and improving care outcomes.
- Options: TensorFlow, PyTorch, Power BI, Tableau.
- Why They Matter: Enable predictive analytics and insights.
With your tech stack chosen, let’s walk through the EHR development process.
EHR Software Development Process
Building an EHR system follows a structured process to ensure functionality, compliance, and user satisfaction. Each phase, from planning to support, requires careful execution to deliver a reliable solution.
Step 1: Discovery & Planning
Begin by gathering requirements through interviews with stakeholders, including clinicians, administrators, and IT staff, to understand their needs and workflows. Identify key features, such as e-prescriptions or telehealth integration, and define compliance requirements like HIPAA or ONC standards. Create a detailed project roadmap with milestones, timelines, and resource allocations to align your team and set clear expectations for development.
Step 2: Design Phase
Design intuitive UI/UX wireframes using tools like Figma or Adobe XD to map out clinician dashboards, patient portals, and administrative interfaces. Develop interactive prototypes to test user flows, ensuring easy navigation for tasks like charting or scheduling. Incorporate accessibility features, such as adjustable fonts or voice navigation, to make your EHR usable for all staff and patients, aligning with compliance needs.
Step 3: Development Phase
Build the frontend with frameworks like React or Angular for responsive interfaces and the backend with Node.js or Django for secure data processing. Implement APIs for integrations, such as lab systems or telehealth platforms, and design data models to handle patient records efficiently, adhering to FHIR standards for interoperability. Ensure secure coding practices to protect sensitive health data.
Step 4: Testing & Compliance
Conduct thorough testing to verify functionality, performance, and security. Run functional tests to ensure features like appointment scheduling work as intended, performance tests to handle high user loads, and security tests to identify vulnerabilities. Perform HIPAA and ONC audits to achieve certification, addressing any compliance gaps to ensure your EHR meets regulatory standards before deployment.
Step 5: Deployment & Support
Deploy your EHR on cloud platforms like AWS for scalability or on-premise servers for control, based on your organization’s needs. Provide comprehensive staff training through workshops or tutorials to ensure smooth adoption. Offer ongoing technical support to address issues, apply updates, and maintain compliance, ensuring your EHR remains reliable and effective post-launch.
Start your EHR development journey with DEVtrust’s healthcare software experts. From FHIR integration to HIPAA compliance, we build scalable systems for the future. Get started
With the development process outlined, let’s address potential challenges in EHR development.
Challenges in EHR Development
EHR development comes with unique obstacles that can impact your project’s success. Understanding these challenges helps you plan effectively and deliver a robust system.
- Interoperability Issues: Integrating with diverse systems like labs or pharmacies is complex. Use FHIR standards and test integrations early to ensure seamless data exchange.
- Legacy System Integration: Connecting with outdated hospital systems can cause delays. Map legacy data structures and use middleware to bridge gaps.
- Regulatory Complexity: Navigating HIPAA, GDPR, and ONC requirements is time-consuming. Consult compliance experts and embed privacy-by-design to streamline audits.
- User Adoption Barriers: Clinicians may resist new systems. Involve end-users in design and provide hands-on training to ease transitions and boost acceptance.
With challenges in mind, let’s explore the estimated costs of developing an EHR system in 2025.
Estimated Development Costs in 2025
Understanding the costs of EHR development helps you budget effectively. Costs vary based on scope, team expertise, and region, with additional expenses for ongoing maintenance.
- Cost Drivers: Feature complexity, team size, and developer rates (e.g., $50-$150/hour in North America vs. $20-$50 in Asia).
- MVP Range: $80,000-$150,000 for core features like charting and scheduling, suitable for small clinics.
- Full-Scale Solution: $250,000+ for advanced features like AI and telehealth, ideal for hospitals.
- Ongoing Costs: Maintenance, updates, and compliance audits cost 15-20% of initial development annually.
With costs clarified, let’s share tips for a successful EHR project.
Tips for a Successful EHR Project
To ensure your EHR project succeeds, follow these practical tips to streamline development and maximize impact.
- Engage End Users from the Start: Involve doctors, nurses, and administrative staff in the planning phase through interviews or focus groups. Their input ensures your EHR aligns with real-world clinical workflows, such as quick charting for busy physicians, reducing resistance, and improving adoption rates.
- Prioritize Intuitive UI/UX Design: Create simple, clinician-friendly interfaces with clear navigation and minimal clicks to perform tasks like viewing patient records. Test designs with users to refine usability, minimizing training time and errors in high-pressure healthcare environments.
- Adopt Agile Methodology: Use agile development to build iteratively, delivering small feature sets for testing and feedback. This approach allows you to adjust to changing requirements, like new compliance rules, and ensures your EHR evolves based on real user needs.
- Build Scalable and Modular Architecture: Design your EHR with a modular structure to support future integrations, such as AI analytics or IoT devices. This ensures your system can scale to handle growing patient data or additional features without requiring a complete overhaul.
- Embed Compliance Early: Incorporate HIPAA, GDPR, and ONC requirements from the design phase, documenting processes like encryption and audit trails. This proactive approach simplifies certification audits and reduces costly rework later in development.
- Test Extensively with Real Scenarios: Simulate real-world clinical scenarios, such as high patient loads or emergency charting, during testing. Use tools like Selenium for automated testing and involve beta testers to identify usability issues, ensuring reliability under pressure.
With these tips, let’s look at future trends shaping EHR development in 2025 and beyond.
Future Trends in EHR Software (2025 and Beyond)
Staying ahead in EHR development requires embracing emerging technologies that enhance functionality and patient care. In 2025, these trends will define the future of EHR systems.
- Predictive Analytics with AI: AI analyzes patient data to predict risks, like diabetes complications, aiding proactive care.
- Blockchain for Patient Identity: Blockchain ensures secure, verifiable patient identities, reducing fraud and enhancing trust.
- Voice and NLP Interfaces: Voice-enabled charting and NLP queries speed up workflows for clinicians.
- Interoperability Mandates: Stricter regulations push FHIR adoption for seamless data sharing across providers.
- IoT and Remote Monitoring: Integration with wearables and IoT devices enables real-time patient monitoring, improving outcomes.
Let’s wrap up with a summary and your next steps.
Conclusion
By following this roadmap, you now understand what it takes to build a compliant, secure, and scalable EHR system in 2025. With the right features, compliant infrastructure, and thoughtful UX, your system becomes a competitive advantage. But success requires the right development partner.
That’s where DEVtrust delivers unmatched value. We specialize in building secure, compliant, and future-ready EHR systems tailored to the real-world needs of healthcare providers, from small clinics to multi-location hospital networks.
Our teams bring deep technical expertise across React, Node.js, FHIR, and cloud platforms, and we embed HIPAA and ONC compliance into every layer of development. With a focus on communication, innovation, and disciplined execution, DEVtrust turns complex healthcare challenges into intuitive, scalable digital solutions. Let us help you build an EHR that keeps pace with technology, regulations, and patient expectations.
Partner with DEVtrust to build an EHR that transforms healthcare delivery. Contact us today to discuss your project, and let our experts create a solution that drives efficiency and improves outcomes in 2025’s healthcare scene.
EHR Software Development: Ultimate Guide 2025
Unlock seamless EHR software development with key components, the latest tech, and compliance insights. Elevate healthcare efficiency now!
Contact Us