The U.S. healthcare IT software market reached $166.83 billion in 2024 and is projected to grow at 15.46% annually through 2030. Sounds promising, right? But what most reports won’t tell you is that a single weak spot in your software architecture or a missed compliance requirement can lead to compromised patient data, regulatory action, and long-term reputational damage.
If you’re a CTO, a HealthTech founder, or a clinic manager tired of outdated systems, you already know the stakes. You need software that protects patient privacy, meets strict regulatory standards, and actually helps your team deliver better care. The good news is that by understanding the essentials of healthcare software development, you can build solutions that are secure, compliant, and aligned with clinical workflows from day one.
That is exactly what this guide helps you do. You’ll learn what sets healthcare software apart from standard applications, the true costs involved, the compliance standards you cannot overlook, and the key decisions that shape a safe, scalable solution. You’ll also understand how to choose a development partner who knows the realities of building for healthcare. Whether you’re planning your first healthcare app or replacing a system that is holding you back, you’ll walk away with a clear roadmap for success.
Key Takeaways
- Plan with Precision: Map workflows, compliance, and integrations before writing a single line of code. Mistakes here cost time, money, and patient trust.
- Build for Reliability: Cloud-native, modular architecture with FHIR and HL7 ensures seamless data flow, real-time performance, and scalability under pressure.
- Design for Users: Interfaces must be intuitive for clinicians, admins, and patients to enable faster adoption and reduce operational friction.
- Embed Compliance Everywhere: HIPAA, GDPR, FDA, and state rules should guide every step, including architecture, security, and deployment.
- Future-Proof Your Software: AI transparency, real-time interoperability, zero-trust security, and integrated patient experiences are now baseline. Partnering with specialists like DEVtrust, who bring pre-built healthcare patterns and compliance expertise, can accelerate your roadmap safely.
What is Modern Healthcare Software Development?
Modern healthcare software development focuses on creating digital systems that align with clinical workflows and enable smooth information flow across departments. The goal is to give providers tools that are reliable, secure, and aligned with everyday operations.
Where Today’s Healthcare Software Functions:
EHR management, telehealth, scheduling, billing, remote monitoring, device connectivity, and care coordination. As digital adoption increases, providers expect platforms that maintain speed, accuracy, and compliance at every touchpoint.
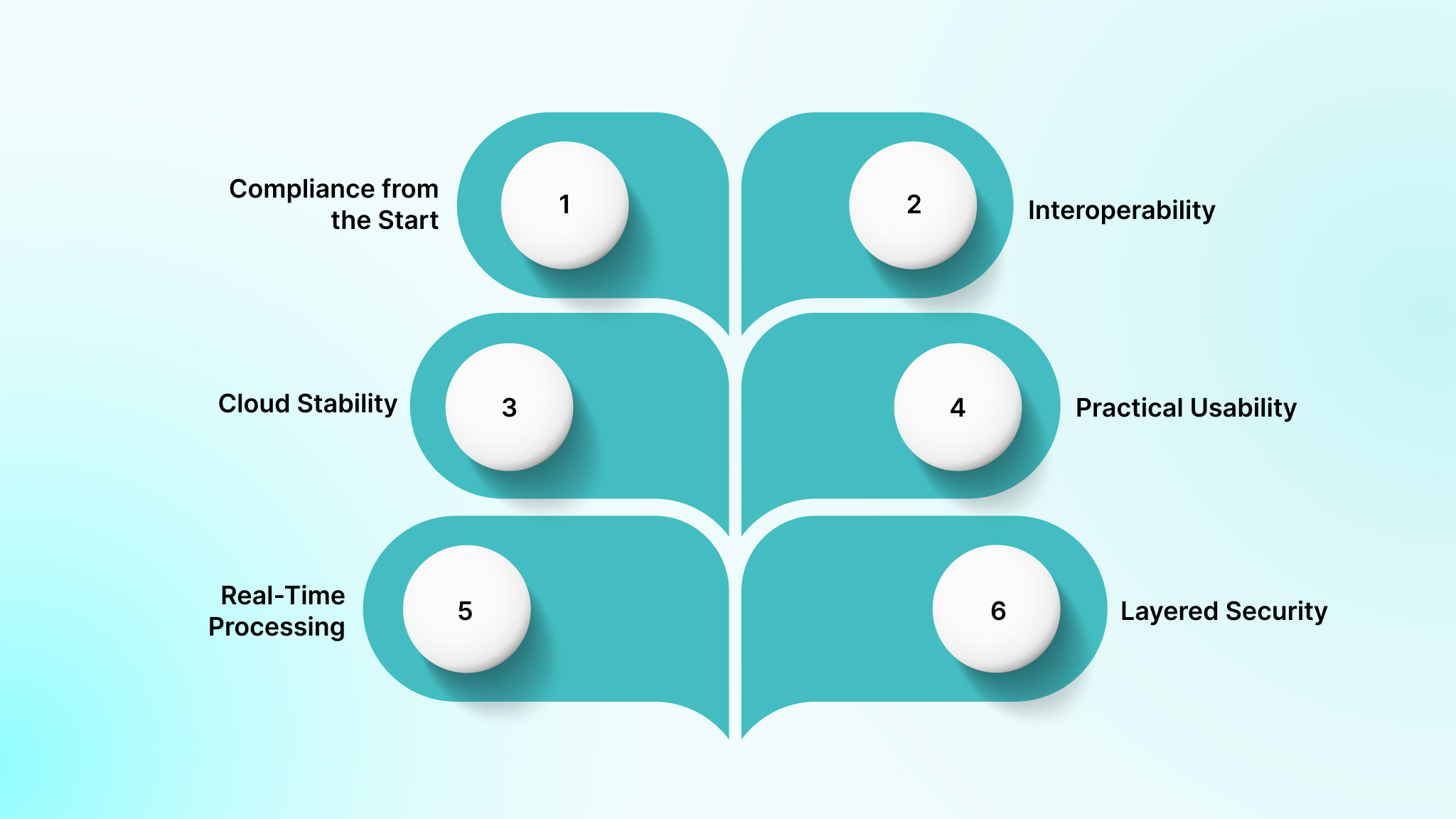
Core Requirements of Effective Healthcare Software:
- Compliance from the Start: HIPAA-based authentication, encryption, access controls, and audit trails.
- Interoperability: Standards such as HL7 FHIR for data exchange with EHRs, labs, imaging systems, billing systems, and insurers.
- Cloud Stability: AWS, Azure, or Google Cloud for secure backups, scalability, and consistent uptime.
- Practical Usability: Clear interfaces that support clinicians, admins, and patients without extra steps.
- Real-Time Processing: Smooth handling of alerts, device data, and monitoring systems.
- Layered Security: Encryption, monitoring, and routine audits to protect sensitive information.
Understanding these elements helps organizations select solutions that support clinical teams effectively and reduce long-term technical challenges.
Types of Healthcare Software Solutions
Healthcare software solutions vary widely, with each type developed to address distinct requirements across clinical, administrative, or operational domains. Let’s examine some common types of Healthcare Software solutions that could be the right fit for you.
| Software Type | Purpose / Benefit |
| Electronic Health Records (EHR) / Electronic Medical Records (EMR) | Centralized digital records of patient health data, including history, diagnoses, medications, and lab results. Enables authorized providers to access and update patient information in real time. |
| Patient Management Systems | Tools for scheduling appointments, tracking patient progress, managing communication, and streamlining front-desk operations. Improves patient flow and administrative efficiency. |
| Telemedicine Platforms | Enable virtual consultations, remote diagnostics, and follow-ups. Expand access to care, especially for rural or underserved populations. |
| Remote Patient Monitoring (RPM) | Collects real-time health data from wearables and IoT devices. Supports chronic disease management and reduces hospital readmissions. |
| Pharmacy Management Systems | Manage medication inventory, prescriptions, refills, and patient safety. Helps prevent medication errors and supports regulatory compliance. |
| Laboratory Information Systems (LIS) | Manage lab workflows, including test ordering, specimen tracking, results reporting, and quality control. Ensures accuracy and efficiency in diagnostics. |
| Radiology Information Systems (RIS) | Handle imaging workflows, including patient scheduling, image storage (PACS integration), AI-powered analysis, and report generation. |
| Clinical Decision Support Systems (CDSS) | Provide evidence-based recommendations and alerts to help healthcare providers make accurate, timely decisions. Reduces diagnostic errors. |
| Billing & Invoicing Modules | Automate patient billing, insurance claims, co-payments, and financial reporting. Improves revenue cycle management and reduces claim denials. |
| Hospital Management Systems (HMS) | Integrate administrative, clinical, financial, and operational functions across departments. Streamline workflows and improve resource allocation. |
| Drug Discovery Systems | Support research and development of new pharmaceuticals using AI, big data, and simulation tools. Accelerate time-to-market for new drugs. |
| AI-Powered Chatbots & Virtual Assistants | Offer 24/7 support for appointment booking, symptom checking, FAQs, and triage. Enhance patient engagement and reduce staff workload. |
Each category demands specific technical capabilities, compliance considerations, and user experience design. Your choice depends on who you’re serving, the workflows you’re supporting, the systems you’re integrating with, and where your organization is strategically headed.
Must-Have Features for User-Centric Healthcare Software
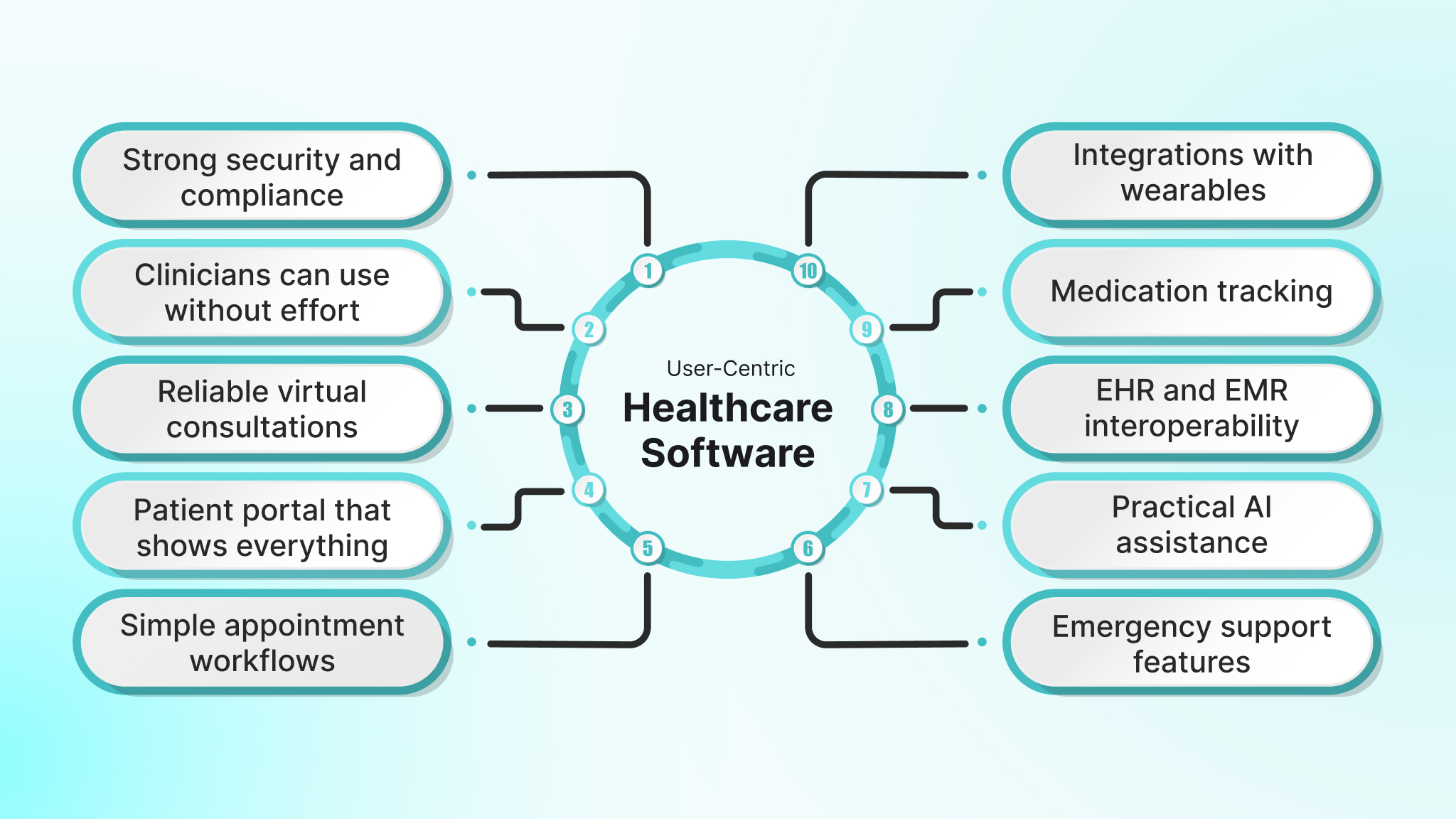
A modern platform must reduce work, maintain accurate information, and support care without slowing anyone down. The list below will help you understand what a current-day system must offer before committing to a vendor, or where your current system is failing.
Strong security and compliance
The software must protect patient records at every step. This includes multi-factor authentication, encryption, role-based access, and detailed activity logs. It should be ready for audits and aligned with major health regulations, without requiring teams to manage security manually.
Interfaces that patients and clinicians can use without effort
The interface should have clear layouts, predictable navigation, and support for screen readers and keyboard controls to make the platform accessible to all users, including those with limited digital experience.
Reliable virtual consultations and communication
Patients expect online care that feels stable and predictable. High-quality video, clear audio, secure messaging, and the ability to share reports or images should be built directly into the platform rather than added as external tools.
A patient portal that shows everything in one place
Patients should not have to switch between systems to view their records, lab results, prescriptions, and upcoming appointments. A single portal should keep them informed and improve follow-through on treatment plans.
Simple appointment workflows
A modern system must allow quick booking, canceling, and rescheduling. Automated reminders, waitlist management, and provider calendar syncing help reduce no-shows and ease clinic coordination.
Integrations with wearables and medical devices
Continuous data from devices such as glucose monitors, blood pressure cuffs, and smartwatches provides clinicians with a clearer picture of patient health. Automatic syncing supports early intervention and more accurate follow-ups.
Medication tracking that supports adherence
The software should help patients keep track of doses, refills, timing, and potential interactions. Consistent guidance reduces errors and supports long-term treatment results.
EHR and EMR interoperability
Clinicians need full context before every visit. The platform must be able to pull and update patient information through standard health data connections, thereby reducing duplicate entry and improving accuracy.
Practical AI assistance
In 2025, AI needs to address fundamental clinical and operational pain points. This includes decision support for clinicians, risk prediction for chronic conditions, documentation support, and forecasting for resource planning.
Emergency support features
Quick access to help matters during critical situations. Location sharing, emergency contact alerts, and direct links to urgent care services should be built into the platform for high-risk users.
When these features are built with your workflows in mind, adoption increases, and administrative work decreases. Evaluate your current systems. If your software doesn’t check these boxes, it may be time to explore a custom solution that reduces friction, improves care, and protects your investment.
Compliance Standards Your Healthcare Software Must Meet
Healthcare software operates in one of the most regulated environments. If your platform mishandles data, lacks audit controls, or fails to meet compliance requirements, the consequences are immediate: fines, legal exposure, stalled launches, and loss of patient trust. Your software must meet specific standards from day one.
Here are the essential compliance areas your solution needs to cover:
- HIPAA (U.S.)
- Risk: PHI exposure leads to financial penalties, mandatory audits, and reputational damage that takes years to repair.
- What your software needs: End-to-end encryption, strict access control, session logging, and full audit trails.
- Next step: Ensure your architecture supports the Privacy, Security, and Breach Notification rules from the beginning.
- HITECH
- Risk: Third-party vendors can expose you to breaches you didn’t cause but are still accountable for.
- What your software needs: Real-time breach monitoring, secure vendor workflows, and documented Business Associate processes.
- Next step: Treat vendor access as part of your core security design.
- GDPR (EU data)
- Risk: If even a portion of your users are in the EU, missing GDPR puts revenue and brand reputation at risk.
- What your software needs: Consent management, data export capability, right-to-erasure workflows, and transparent data handling.
- Next step: Map out where EU user data lives and ensure your system supports GDPR rights natively.
- FDA Considerations for SaMD
- Risk: Software used in diagnosis or treatment may require formal FDA review; skipping this halts launches and triggers rework.
- What your software needs: documentation, validation, test evidence, risk controls, and lifecycle processes that match SaMD rules.
- Next step: Classify your software early to avoid delays and rebuilds later.
- HL7 & FHIR Interoperability
- Risk: Non-standard integrations cause data inconsistencies, duplicate work, and poor clinical workflows.
- What your software needs: Support for FHIR APIs, structured data formats, and clean integration pathways with EHRs and external systems.
- Next step: Confirm your development roadmap includes FHIR-native interfaces, not custom, ad hoc integrations.
- State-Level Privacy Requirements
- Risk: Telehealth, consent rules, and privacy laws vary by state, and missing any of them can result in fines or delayed deployments.
- What your software needs: Configurable privacy controls, location-based data rules, and adaptable consent flows.
- Next step: Review the regulatory conditions for every region you plan to operate in.
- Quality & Risk Management Standards
- Risk: Clinical software without a defined lifecycle and risk controls fails audits and becomes impossible to scale safely.
- What your software needs: Processes aligned with standards such as IEC 62304 (software lifecycle), ISO 14971 (risk management), and ISO 13485 or ISO 9001 (quality management), including traceability from requirements to tests.
- Next step: Ask your development team for traceability matrices, risk logs, and quality documentation that map directly to these frameworks.
Compliance shapes every part of your software journey. When you get it right, you reduce delays, protect patient trust, and scale confidently. This is why it’s critical to work with teams who have done this before.
At DEVtrust, we help healthcare organisations align engineering, security, and documentation practices with HIPAA, GDPR, FDA, and interoperability standards so you can ship audit-ready systems without constant rework.
Healthcare Software Development Process: Step by Step
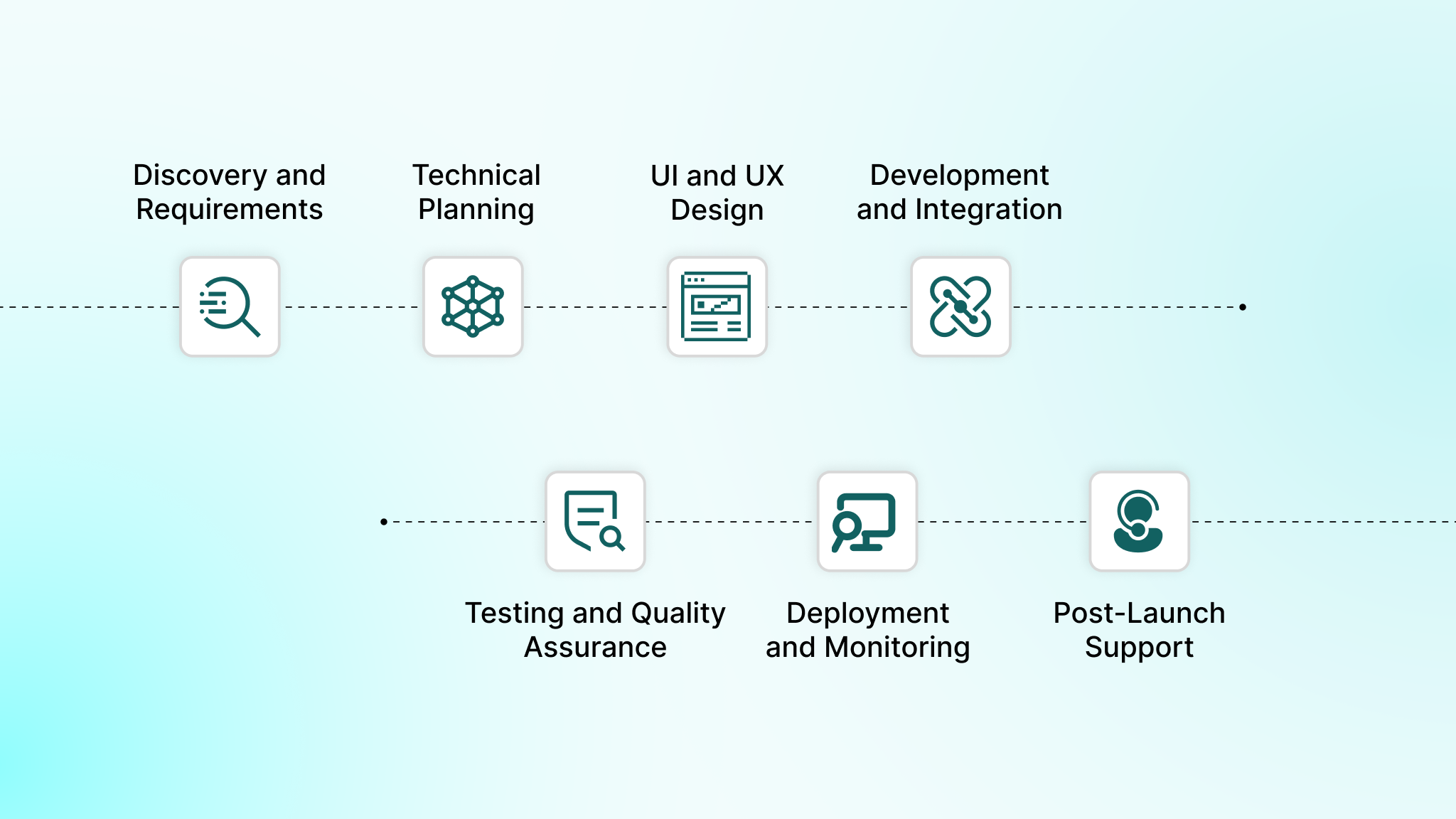
Building healthcare software is all about striking a balance between speed and quality, innovation and compliance, and functionality and security. Because clinical workflows and patient data are involved, every step requires careful planning and execution.
Here’s how a modern, reliable healthcare software product comes to life:
Step 1: Discovery and Requirements
Many software projects fail because they don’t align with real-world clinical workflows, resulting in frustration and inefficiency. In the discovery phase, teams gather clarity before writing a single line of code.
Key activities:
- Interview clinicians, administrators, and staff to identify workflow gaps.
- Define functional requirements that specify exactly what the system must do.
- Establish non-functional requirements for performance, reliability, and scalability.
- Map compliance needs based on HIPAA, GDPR, and local regulations.
- Assess existing systems to plan integrations and data migration.
Taking the time to understand workflows and compliance early ensures smoother adoption and reduces costly rework later.
Step 2: Architecture and Technical Planning
A solid technical foundation prevents future slowdowns, errors, and security risks.
Key activities:
- Select tech stack based on scalability & compliance (e.g., Node.js/Java/.NET with React/Angular + cloud-native architecture).
- Design a zero-trust, HIPAA-aligned architecture with RBAC, MFA, end-to-end encryption, audit trails, and tokenization.
- Define interoperability standards (FHIR R4, HL7v2, DICOM) for integrations.
- Architect microservices, event-driven systems, or modular monoliths depending on scale.
- Plan databases using normalized schemas for PHI and time-series data for vitals, and separate audit tables.
- Prepare infrastructure using IaC (Terraform), container orchestration (Kubernetes), and automated CI/CD pipelines.
- Define SLAs and load thresholds, throughput, downtime tolerance, and horizontal scaling strategies.
Proper planning here protects patient data, maintains system performance, and reduces operational risks.
Step 3: UI and UX Design
Even the most powerful software fails if users struggle with it. The design phase ensures clinicians and patients can navigate the platform effortlessly.
Key activities:
- Create low-fidelity wireframes → high-fidelity prototypes using Figma.
- Define interaction models for high-density screens (EHRs, dashboards, imaging viewers).
- Simulate workflows: charting, order sets, lab/radiology flows, telehealth, and medication management.
- Conduct usability testing with clinicians using heuristic analysis and task-completion metrics.
- Apply healthcare-specific UX principles: hierarchy for clinical urgency, color-coded alerts, and predictable navigation.
- Ensure WCAG 2.1 accessibility compliance.
Intuitive interfaces increase adoption, reduce training time, and make clinical work faster and safer.
Step 4: Development and Integration
This is where the product begins to take shape. Agile development enables teams to build, test, and adjust in short, iterative cycles.
Key activities:
- Implement modular front-end components optimized for fast interaction workflows.
- Build back-end services for authentication, care flows, clinical rules, scheduling logic, billing logic, etc.
- Integrate with EHR/EMR systems using FHIR APIs, HL7v2 messages, CCD/CDA documents, or custom integration engines.
- Build secure API gateways + rate limiting + JWT/OAuth2.
- Implement event logging, audit tracking, and PHI encryption at rest (AES-256) and in transit (TLS 1.2+).
- Configure cloud infrastructure (AWS/GCP/Azure) with HIPAA-aligned environments.
Integration with existing systems ensures data consistency and a seamless user experience.
Step 5: Testing and Quality Assurance
Healthcare software must be flawless; errors can significantly impact patient outcomes, compliance, and operational efficiency.
Key activities:
- Functional testing using automated test suites + manual edge-case validation.
- Penetration testing for PHI exposure risks, API vulnerabilities, and authentication loopholes.
- Performance/load testing simulating peak clinical hours.
- Integration testing to ensure clean data flow between EHRs, labs, imaging, and billing.
- Regression testing through CI pipelines.
- Validation testing to verify workflows match real-world clinical use cases.
Thorough testing avoids costly post-launch fixes and ensures staff can trust the platform.
Step 6: Deployment and Monitoring
Deployment is done with zero downtime and full observability.
Key Technical Activities:
- Deploy to HIPAA-compliant cloud environments using blue-green or canary releases.
- Set up real-time monitoring (APM, logs, metrics) using tools like Datadog, Elastic, Prometheus, or CloudWatch.
- Configure automated alerts for unusual access, performance drops, or API failures.
- Implement incident response plans (24/7 escalation, breach response workflows).
- Validate access roles, audit logs, and encryption keys before go-live.
Monitoring and careful deployment keep the system stable, secure, and reliable from day one.
Step 7: Post-Launch Support and Iteration
Healthcare software evolves as regulations change and clinical needs grow. Ongoing support ensures it continues to deliver value.
Key activities:
- Release security patches, compliance updates, and feature upgrades through CI/CD.
- Capture telemetry data and analyze usage patterns to optimize workflows.
- Expand modules (e.g., telehealth, chronic care, pharmacy, imaging, billing).
- Conduct periodic penetration tests + HIPAA risk assessments.
- Update integration engines as partner systems change (e.g., new FHIR endpoints).
- Manage version upgrades and backward compatibility.
Continuous improvement keeps teams productive, patients safe, and software aligned with changing requirements.
Now, even the clearest process can go off track if steps aren’t executed properly, leading to compliance gaps, broken integrations, and frustrated clinical users.
Common Roadblocks in Healthcare Software Development (and How You Can Avoid Them)

Even with the right idea and budget, healthcare software projects get stuck for reasons that aren’t obvious at the start. You’ve likely dealt with some of these already: compliance surprises, unstable integrations, performance issues, or workflows that look good on paper but break in real clinical environments.
Below are the real roadblocks you’ll face, and how to design your product and your development workflow to avoid them from day one.
1. Regulatory Compliance Gaps That Surface Too Late
HIPAA, GDPR, state privacy rules, and FDA expectations each have overlapping and sometimes conflicting requirements. Teams often map functional features correctly but miss compliance dependencies until code is already written.
How to avoid it
- Bring a compliance specialist into your requirements and design conversations, not only during QA.
- Document each compliance decision with the specific regulation it maps to.
- Add compliance checks to architecture reviews, not just testing cycles.
- Maintain a dynamic compliance register to track changes in standards.
- Run periodic external audits to catch blind spots early.
If your development partner cannot speak confidently about HIPAA implementation specifics, access controls, audit readiness, and FDA implications, that’s a red flag.
2. Fragile Integrations With Legacy Systems
Most hospitals rely on older EHRs, imaging tools, billing systems, and lab interfaces. These systems often use outdated HL7 versions, inconsistent implementations, or custom interfaces that fail under load.
How to avoid it
- Map every interface, event trigger, and dependency before writing any code.
- Use integration engines like Mirth Connect for transforming HL7, FHIR, CCD, and custom formats.
- Add retry logic and clear error reporting for unstable interfaces.
- Build a full staging environment that mirrors production-level integrations.
- Implement fallback behaviors when external systems drop or time out.
If your team or vendor can’t show you an integration strategy upfront, the risk of downtime and workflow disruption increases dramatically.
3. Workflow Misalignment That Slows Down Clinicians
A system that looks efficient to engineers can break the rhythm of clinicians who work under time pressure and handle dozens of edge cases every day.
How to avoid it
- Spend time observing real clinical workflows across shifts; the exceptions matter more than the rule.
- Involve clinicians in prototype reviews, not after development.
- Add configuration options for variations across units, facilities, and roles.
- Conduct role-specific training sessions before rollout.
- Treat workflow feedback as an ongoing development input, not a one-time step.
If users struggle in the first week, adoption collapses and your investment loses momentum fast.
4. Security Vulnerabilities Hidden in Code and Configurations
Healthcare is the most targeted industry for cyberattacks. One misconfigured API, an outdated library, or a missing access control can expose thousands of records.
How to avoid it
- Use layered security with RBAC, MFA, and least-privilege access.
- Automate security checks in CI/CD to block risky builds.
- Run scheduled penetration tests, SAST, and dependency scans.
- Maintain a real incident response plan with defined escalation paths.
- Train technical and clinical teams on real-world threat scenarios.
If your software handles PHI, you need continuous verification.
5. Scalability and Performance Bottlenecks Under Real-World Loads
Healthcare traffic is unpredictable. Appointment surges, seasonal peaks, and operational spikes can break systems that performed perfectly in test environments.
How to avoid it
- Choose cloud-native architecture for automatic scaling.
- Run load tests modeled on peak-day traffic patterns, not averages.
- Add intelligent caching to reduce database load.
- Track performance metrics continuously and prioritize fixes for bottlenecks.
- Allocate capacity with headroom for clinical surges.
A system that lags during peak hours causes delays, frustrated staff, and operational risks.
6. Budget and Timeline Overruns Caused by Late Surprises
Most healthcare projects run over budget because of underestimated compliance work, late architectural changes, and scope creep.
How to avoid it
- Build timelines that include compliance cycles, security reviews, and integration delays.
- Deliver in feature-based phases so essential modules go live early.
- Enforce a formal change request process to manage scope.
- Add a buffer for regulatory or integration surprises.
- Review progress frequently and adjust plans before delays escalate.
A disciplined plan up front saves months of rework later.
Knowing the hurdles is one thing, but planning your budget around them is another. Understanding the costs involved ensures you allocate resources wisely and choose the development path that delivers measurable ROI.
How Much Does Custom Healthcare Software Cost?
Investing in custom healthcare software is a strategic decision: it reduces administrative work, improves patient outcomes, and protects revenue. Knowing what to expect upfront helps you avoid surprises and make informed choices.
Why Costs Vary
The total investment depends on your organization’s size, workflow complexity, and the number of integrations required. Prioritizing the right features and rolling out development in phases ensures a predictable budget and measurable ROI.
Typical Cost by Development Phase
| Phase | Typical Cost | Timeline | What Drives Cost |
| Discovery & Planning | $15,000 – $50,000 | 2–6 weeks | Stakeholder interviews, workflow mapping, compliance assessment |
| UI/UX Design | $20,000 – $60,000 | 3–8 weeks | Number of user roles, workflow complexity, accessibility requirements |
| Core Development | $100,000 – $400,000 | 3–12 months | Feature scope, integrations, workflow automation |
| Testing & QA | $25,000 – $80,000 | 3–6 weeks | Security validation, performance testing, and regulatory compliance |
| Deployment & Training | $10,000 – $40,000 | 2–4 weeks | Staff onboarding, infrastructure setup |
| Annual Maintenance | 15–25% of the development cost | Ongoing | Updates, compliance monitoring, system optimization |
Key Cost Drivers
- Regulatory Compliance – Ensuring compliance with HIPAA, FDA, and state-level regulations is non-negotiable. Integrating security, audit logs, and privacy controls upfront reduces long-term risks.
- Integration Complexity – Connecting EHRs, labs, imaging systems, and insurance networks adds time and requires specialized expertise.
- Feature Set – Scheduling, telehealth, patient portals, analytics, and automation tools increase development scope but drive ROI.
- Mobile & Web Access – Native mobile apps improve adoption and usability; cross-platform development can reduce cost while maintaining performance.
ROI You Can Expect
When deployed thoughtfully, custom healthcare software delivers solid, measurable results within 18–30 months:
You can typically see:
- 30-50% reduction in documentation time.
- 20-35% faster claim processing and reimbursement.
- 15-25% decrease in administrative labor costs.
- 25-40% improvement in patient satisfaction scores.
With a solid grasp of core requirements, the development team can plan effectively and avoid costly missteps. Next, let’s look at 2026 trends to make you aware of what should be the core of your software.
2026 Healthcare Software Trends You Should Prepare For
As you plan your 2026 roadmap, you need to build in operational and technical shifts to your healthcare software architecture now, whether you’re guiding an internal team or evaluating an external development partner.
Let’s examine the important trends:
1. AI-Driven Clinical Automation Will Require Transparent, Traceable Systems
AI is finally moving past experimentation and into clinical workflows, triage automation, risk scoring, diagnostics, and care coordination. But in 2026, regulators are expected to push for explainable AI (XAI), making transparency non-negotiable.
What this means for your software:
- Your models must support audit-ready decision logs, including confidence scores and reasoning trails.
- You’ll need governance around model versioning, drift monitoring, and bias checks.
- Any AI features must integrate with your EHR using FHIR Subscriptions, not legacy HL7 polling.
- If you’re building predictive tools, ensure your stack supports GPU-optimized microservices to prevent inference from slowing down clinical operations.
If your software uses AI, make sure your development partner can implement, monitor, and clinical audit pathways; these will be required, not optional.
2. FHIR 5 Adoption and Real-Time Interoperability Will Become a Competitive Advantage
With more payers, providers, and state-level systems moving toward FHIR R5 in 2026, you’ll be expected to support real-time data exchange, not delayed syncs or batched updates.
What this means for your software:
- Shift from a monolithic architecture to an event-driven microservices architecture so your system can publish/subscribe to clinical events in real time.
- Build with FHIR R5 resources, especially for medication reconciliation, scheduling, and care planning.
- Implement bulk data APIs for population analytics, quality reporting, and payer-provider data contracts.
- Ensure your backend supports asynchronous messaging (Kafka, NATS, or Pub/Sub) to avoid blocking clinical tasks.
If you’re evaluating a custom development team, make sure they can build systems that use FHIR subscriptions, bulk exports, and event triggers — this is how you prevent workflow delays and data mismatches.
3. Cybersecurity Will Shift From “Protection” to “Continuous Verification”
Cyberattacks on healthcare will keep climbing, and in 2026, you’re going to see regulatory pressure for zero-trust, continuous authentication, and real-time anomaly detection.
What this means for your software:
- Implement role-based access with continuous authentication, not static session tokens.
- Encrypt PHI both in transit and at rest using TLS 1.3 and AES-256 by default.
- Add behavioral analytics to detect unusual access patterns (e.g., sudden bulk downloads).
- Build isolated PHI microservices so a breach in one module doesn’t expose the entire system.
- Ensure incident response pipelines include automated threat logs that tie directly into SIEM tools.
Ask your dev team whether they can build systems with zero-trust gating, privileged access workflows, and automated PHI security audits; these are now baseline requirements.
4. Patient-Facing Experiences Will Move Toward Integrated, Multi-Modal Care
2026 will push patient platforms beyond basic portals. You’ll need systems that support telehealth, remote diagnostics, wearable data ingestion, and automated follow-ups, all in one cohesive experience.
What this means for your software:
- Support real-time device data ingestion using MQTT, WebSockets, or vendor SDKs.
- Build care plans that adapt using rules engines and AI-assisted decision support.
- Integrate telehealth, scheduling, medication management, and patient messaging into a single interface rather than fragmented apps.
- Ensure accessibility and ADA compliance across all patient-facing modules.
If you’re commissioning a new patient experience, ensure your partner can build multi-modal care flows that operate seamlessly across desktop, mobile, and connected devices.
5. Virtual Care Infrastructure Will Demand High-Performance Systems
In 2026, virtual care will require low-latency streaming, automated documentation, and integrated diagnostics.
What this means for your software:
- Use WebRTC-based video with adaptive bitrate and HIPAA-ready configurations.
- Integrate AI-driven SOAP auto-documentation to reduce clinician workload.
- Add remote diagnostic tools (vitals ingestion, device pairing, image capture).
- Optimize your backend for <200 ms latency during peak hours.
If you’re scaling virtual care, your engineering partner must understand HIPAA-compliant streaming, edge computing, and AI documentation pipelines.
These 2026 trends make it clear: building modern healthcare software requires technical depth, regulatory foresight, and alignment with workflows. The next critical decision is choosing how to execute: should your organization build internally or partner with an experienced development team? Let’s see.
In-House Development vs. Outsourcing: Which Path Leads to Success?
Choosing how to develop your healthcare software is one of the most strategic decisions you will make. Both in-house development and outsourcing have merits, but the right approach depends on your resources, timelines, and compliance requirements.
In-House Development: Control Comes at a Cost
Building software internally gives you control over priorities, processes, and intellectual property. Your developers immerse themselves in your organization’s culture and workflows, and communication happens naturally.
However, in healthcare contexts, internal teams face significant challenges:
- Recruitment challenges: Hiring developers with healthcare domain expertise can take months and often competes with well-funded tech companies for scarce talent.
- Compliance complexity: Building HIPAA-compliant systems, mastering FDA regulations, and implementing secure data protocols require years of experience. Mistakes can be costly.
- Technical specialization: Integrating with HL7 FHIR standards, medical devices, and EHR systems demands niche skills. These capabilities take time and money to develop, delaying your project.
- Hidden costs: Salaries, benefits, onboarding, training, and retention for skilled healthcare software developers often exceed the cost of outsourcing these services.
Even with a capable internal team, projects risk delays, cost overruns, and compliance missteps.
Outsourcing: Expertise On-Demand
Specialized healthcare software development partners bring experience solving these exact problems. They have built HIPAA-compliant systems, navigated FDA approvals, integrated with EHR platforms, and optimized clinical workflows.
The benefits include:
- Faster timelines: Proven frameworks and experienced teams reduce development cycles.
- Lower risk: Expertise in compliance and integration helps avoid costly mistakes.
- Flexible scaling: Pay for the capacity you need, ramping up for development phases and scaling down during maintenance.
- Cross-industry insights: Exposure to multiple healthcare organizations ensures solutions that are practical, user-friendly, and scalable across various settings.
- Cost efficiency: Outsourcing eliminates high salaries, training, and infrastructure costs associated with maintaining an internal team of specialized healthcare developers.
Choosing the Right Partner
To maximize results, look for outsourcing teams with:
- A strong portfolio of healthcare projects similar to yours.
- Deep compliance knowledge and documentation practices.
- Transparent communication and agile workflows.
- Support for long-term maintenance beyond initial deployment.
Outsourcing doesn’t mean giving up control; it means leveraging specialized expertise so you can focus internal resources on strategic initiatives. Many organizations find that this approach delivers projects faster, within budget, and with higher-quality outcomes than building in-house.
How DEVtrust Helps You Deliver Reliable, Risk-Free Healthcare Software?
When you outsource your healthcare software development, the biggest risk is partnering with a team that is still learning healthcare as they go. You need engineers who already understand clinical workflows, regulatory pressure, and the operational reality inside hospitals, clinics, and HealthTech platforms.
At DEVtrust, we specialise in building secure, compliant healthcare systems for U.S. organisations. We help you handle timelines, integrations, and compliance end-to-end so you’re not forced to manage every technical decision alone.
Here is what that partnership will look like for you:
- You will receive structured discovery and planning that surfaces hidden risks early, helping you avoid delays, scope creep, and last-minute redesigns.
- Your compliance requirements remain under control throughout the project because HIPAA, HITECH, encryption standards, access controls, and audit requirements are integrated from the start.
- Your integrations work cleanly, whether you’re connecting to EHRs, labs, credentialing systems, or third-party healthcare APIs. You don’t end up with data silos or fragile connections.
- Your team experiences real workflow improvements because design decisions are based on observing how clinicians and administrators actually work, not on assumptions.
- Your platform scales predictably, built on cloud architecture and modular components that handle growth without sacrificing performance.
- You avoid unnecessary complexity by keeping communication steady, explanations clear, and milestones visible, thereby reducing operational pressure on your team.
- You maintain long-term stability with ongoing support for compliance updates, new features, performance improvements, and long-term product evolution.
And these aren’t theoretical promises; you can see similar outcomes in recent DEVtrust projects:
- With Precina, you can see how structured automation and secure data handling reduced manual operational tasks by nearly 98%, improved document accuracy, and strengthened user trust through secure OTP-based login.
- With the Spero Institute, you can see how a patient-clinician platform creates smoother coordination, secure role-based access, measurable therapy progress tracking, and video session support, giving their team a more transparent and productive digital workflow.
These examples reflect the kind of partnership you experience with DEVtrust: practical, predictable, and aligned with how healthcare actually operates.
When your responsibility is to deliver a secure, compliant, and high-performing product, having the right development partner makes all the difference. With DEVtrust, you move forward with a team that protects your time, reduces your risk, and helps you build software that truly supports your organization.
Conclusion
By now, you have a clear view of what it truly takes to build healthcare software that works in real clinical settings. The next step is choosing a team that can translate your goals into a dependable product without slowing you down. Effective healthcare software development is not only about writing code. It is about aligning your vision with the right strategy, architecture, security approach, and execution.
This is where Devtrust adds real value. We work with healthcare teams who want clarity, speed, and reliable delivery. If you need a partner who understands compliance, handles the technical depth, and keeps your build moving in the right direction, we are here to help.
If you are ready to move from planning to building, let’s talk.